Dosing & Uses
Dosage Forms & Strengths
tablet
- 10mg
- 20mg
- 30mg
- 40mg
capsule
- 7.5mg
tablet, extended-release
- 12.5mg
- 25mg
- 37.5mg
oral suspension
- 10mg/5mL
Depression
Conventional: 20 mg PO qDay initially; may increase by 10 mg/day qWeek not to exceed 50 mg/day
Paxil CR: 25 mg PO qDay initially; may increase by 12.5 mg/day qWeek not to exceed 62.5 mg/day
Obsessive-Compulsive Disorder
20 mg PO qDay initially; may increase by 10 mg qWeek, not to exceed 60 mg/day
Panic Disorder
10 mg PO qDay initially; may increase by 10 mg qWeek (target dose 40 mg/day), not to exceed 60 mg/day, OR
Paxil CR: 12.5 mg PO qDay initial, increase by 12.5 mg qWeek not to exceed 75 mg/day
Social Phobia
20 mg PO qDay OR
Paxil CR: 12.5 mg PO qDay initially; may increase by 12.5 mg qWeek, not to exceed 37.5 mg/day
Generalized Anxiety Disorder
20 mg PO qDay initially, may increase by 10 mg qWeek, up to 50 mg/day doses have been used but no increase in benefit seen at doses >20 mg/day
Posttraumatic Stress Disorder
20 mg PO qDay initially; may increase by 10 mg qWeek, up to 50 mg/day doses have been used but no increase in benefit seen at doses >20 mg/day
Premenstrual Dysphoric Disorder
Paxil CR: 12.5 mg PO qDay initially; may increase at 1 week intervals not to exceed 25 mg/day
Menopausal Vasomotor Symptoms
Brisdelle: Indicated to treat moderate-to-severe vasomotor symptoms associated with menopause
Brisdelle: 7.5 mg PO qHS
Paxil CR (Off-label): 12.5-25 mg PO qDay
Dosing Modifications
Severe renal impairment (CrCl <30 mL/min)
- Conventional: 10 mg PO qDay initially; may titrate; not to exceed 40 mg/day
- Paxil CR: 12.5 mg PO qDay initially; may titrate; not to exceed 50 mg/day
Stuttering (Off-label)
20 mg PO qDay
Vasovagal Syncope (Off-label)
20 mg/day PO
Diabetic Neuropathy (Off-label)
10 mg/day PO initially; may increase to 20-60 mg/day
Safety and efficacy not established
Caution should be used in the elderly because paroxetine is the most sedating and anticholinergic of the selective serotonin reuptake inhibitors
The elderly are prone to SSRI/SNRI-induced hyponatremia; monitor closely
Interactions
Interaction Checker
No Results

Contraindicated
Serious - Use Alternative
Significant - Monitor Closely
Minor

Contraindicated (8)
- eliglustat
paroxetine increases levels of eliglustat by affecting hepatic enzyme CYP2D6 metabolism. Contraindicated. If coadministered with strong or moderate CYP2D6 inhibitors, reduce eliglustat dose from 84 mg BID to 84 mg once daily in extensive and intermediate metabolizers; eliglustat is contraindiated if strong or moderate CYP2D6 inhibitors are given concomitantly with strong or moderate CYP3A inhibitors.
- isocarboxazid
isocarboxazid and paroxetine both increase serotonin levels. Contraindicated.
- phenelzine
phenelzine and paroxetine both increase serotonin levels. Contraindicated.
- pimozide
paroxetine increases levels of pimozide by affecting hepatic enzyme CYP2D6 metabolism. Contraindicated. Contraindicated. Coadministration increases pimozide AUC and Cmax and may result in prolonged QT interval.
- procarbazine
procarbazine and paroxetine both increase serotonin levels. Contraindicated. Combination is contraindicated within 2 weeks of MAOI use.
- selegiline
selegiline and paroxetine both increase serotonin levels. Contraindicated. At least 14 days should elapse between discontinuation of selegiline and initiation of treatment with a serotonergic drug.
- thioridazine
paroxetine increases levels of thioridazine by decreasing metabolism. Contraindicated. Risk of long QT syndrome.
- tranylcypromine
tranylcypromine and paroxetine both increase serotonin levels. Contraindicated.
Serious - Use Alternative (101)
- alfentanil
alfentanil, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug.
- amiodarone
amiodarone and paroxetine both increase QTc interval. Avoid or Use Alternate Drug.
- amitriptyline
paroxetine and amitriptyline both increase serotonin levels. Avoid or Use Alternate Drug.
- amoxapine
paroxetine and amoxapine both increase serotonin levels. Avoid or Use Alternate Drug.
- aripiprazole
paroxetine will increase the level or effect of aripiprazole by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- arsenic trioxide
arsenic trioxide and paroxetine both increase QTc interval. Avoid or Use Alternate Drug.
- asenapine
asenapine and paroxetine both increase QTc interval. Avoid or Use Alternate Drug.
- asenapine transdermal
asenapine transdermal and paroxetine both increase QTc interval. Avoid or Use Alternate Drug.
- buprenorphine subdermal implant
buprenorphine subdermal implant and paroxetine both increase QTc interval. Avoid or Use Alternate Drug.
- bupropion
bupropion will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
paroxetine increases toxicity of bupropion by unspecified interaction mechanism. Avoid or Use Alternate Drug. May lower seizure threshold; keep bupropion dose as low as possible. - buspirone
paroxetine and buspirone both increase serotonin levels. Avoid or Use Alternate Drug.
- carvedilol
paroxetine will increase the level or effect of carvedilol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- chlorpromazine
paroxetine will increase the level or effect of chlorpromazine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- citalopram
citalopram and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug. Combination may increase risk of serotonin syndrome or neuroleptic malignant syndrome-like reactions.
- clomipramine
paroxetine will increase the level or effect of clomipramine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
paroxetine and clomipramine both increase serotonin levels. Avoid or Use Alternate Drug. - cyclobenzaprine
paroxetine and cyclobenzaprine both increase serotonin levels. Avoid or Use Alternate Drug.
- dacomitinib
dacomitinib will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug. Avoid use with CYP2D6 substrates where minimal increases in concentration of the CYP2D6 substrate may lead to serious or life-threatening toxicities.
- desipramine
paroxetine will increase the level or effect of desipramine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
paroxetine and desipramine both increase serotonin levels. Avoid or Use Alternate Drug. - desvenlafaxine
paroxetine and desvenlafaxine both increase serotonin levels. Avoid or Use Alternate Drug.
- dextromethorphan
paroxetine will increase the level or effect of dextromethorphan by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
paroxetine and dextromethorphan both increase serotonin levels. Avoid or Use Alternate Drug. - disopyramide
disopyramide and paroxetine both increase QTc interval. Avoid or Use Alternate Drug.
- dolasetron
dolasetron, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug.
- dosulepin
paroxetine and dosulepin both increase serotonin levels. Avoid or Use Alternate Drug.
- doxepin
paroxetine will increase the level or effect of doxepin by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
paroxetine and doxepin both increase serotonin levels. Avoid or Use Alternate Drug. - duloxetine
paroxetine will increase the level or effect of duloxetine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
duloxetine and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug. - eliglustat
eliglustat and paroxetine both increase QTc interval. Avoid or Use Alternate Drug.
- escitalopram
escitalopram and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug.
- fedratinib
paroxetine will increase the level or effect of fedratinib by Other (see comment). Avoid or Use Alternate Drug. Avoid coadministration of fedratinib (a CYP3A4 and CYP2C19 substrate) with dual CYP3A4 and CYP2C19 inhibitor. Effect of coadministration of a dual CYP3A4 and CYP2C19 inhibitor with fedratinib has not been studied.
- fentanyl
fentanyl, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug.
- fentanyl intranasal
fentanyl intranasal, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug.
- fentanyl transdermal
fentanyl transdermal, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug.
- fentanyl transmucosal
fentanyl transmucosal, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug.
- flecainide
paroxetine will increase the level or effect of flecainide by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- fluoxetine
fluoxetine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
fluoxetine and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug. - fluphenazine
paroxetine will increase the level or effect of fluphenazine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
fluphenazine and paroxetine both increase QTc interval. Avoid or Use Alternate Drug. - fluvoxamine
fluvoxamine and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug.
- gilteritinib
gilteritinib will decrease the level or effect of paroxetine by Other (see comment). Avoid or Use Alternate Drug. Coadministration of gilteritinib with drugs that inhibit 5HT2B or sigma nonspecific receptors. Avoid use of these drugs with gilteritinib unless coadministration is necessary.
gilteritinib and paroxetine both increase QTc interval. Avoid or Use Alternate Drug. - givosiran
givosiran will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug. Avoid coadministration of sensitive CYP2D6 substrates with givosiran. If unavoidable, decrease the CYP2D6 substrate dosage in accordance with approved product labeling.
- granisetron
granisetron, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug.
granisetron and paroxetine both increase QTc interval. Avoid or Use Alternate Drug. - haloperidol
paroxetine will increase the level or effect of haloperidol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- hydromorphone
paroxetine will increase the level or effect of hydromorphone by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
hydromorphone, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug. - ibutilide
ibutilide and paroxetine both increase QTc interval. Avoid or Use Alternate Drug.
- iloperidone
paroxetine will increase the level or effect of iloperidone by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- imipramine
paroxetine will increase the level or effect of imipramine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
paroxetine and imipramine both increase serotonin levels. Avoid or Use Alternate Drug. - indapamide
indapamide and paroxetine both increase QTc interval. Avoid or Use Alternate Drug.
- levomilnacipran
levomilnacipran and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug.
- linezolid
linezolid and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug. Linezolid may increase serotonin as a result of MAO-A inhibition. If linezolid must be administered, discontinue serotonergic drug immediately and monitor for CNS toxicity. Serotonergic therapy may be resumed 24 hours after last linezolid dose or after 2 weeks of monitoring, whichever comes first.
- lofepramine
paroxetine will increase the level or effect of lofepramine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
paroxetine and lofepramine both increase serotonin levels. Avoid or Use Alternate Drug. - lonafarnib
paroxetine will increase the level or effect of lonafarnib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Avoid or Use Alternate Drug. If coadministration of lonafarnib (a sensitive CYP3A substrate) with weak CYP3A inhibitors is unavoidable, reduce to, or continue lonafarnib at starting dose. Closely monitor for arrhythmias and events (eg, syncope, heart palpitations) since lonafarnib effect on QT interval is unknown.
- lorcaserin
paroxetine and lorcaserin both increase serotonin levels. Avoid or Use Alternate Drug.
- maprotiline
paroxetine and maprotiline both increase serotonin levels. Avoid or Use Alternate Drug.
- mefloquine
mefloquine increases toxicity of paroxetine by QTc interval. Avoid or Use Alternate Drug. Mefloquine may enhance the QTc prolonging effect of high risk QTc prolonging agents.
- meperidine
paroxetine and meperidine both increase serotonin levels. Avoid or Use Alternate Drug.
meperidine, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug. - methamphetamine
paroxetine will increase the level or effect of methamphetamine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- methylene blue
methylene blue and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug. Methylene blue may increase serotonin as a result of MAO-A inhibition. If methylene blue must be administered, discontinue serotonergic drug immediately and monitor for CNS toxicity. Serotonergic therapy may be resumed 24 hours after last methylene blue dose or after 2 weeks of monitoring, whichever comes first.
- metoclopramide
metoclopramide and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug. Additive effects; increased risk for serotonin syndrome, neuroleptic malignant syndrome, dystonia, or other extrapyramidal reactions
- metoclopramide intranasal
paroxetine will increase the level or effect of metoclopramide intranasal by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug. Concurrent use of metoclopramide intranasal and strong CYP2D6 inhibitors is not recommended since the metoclopramide intranasal dose cannot be adjusted.
paroxetine, metoclopramide intranasal. Either increases effects of the other by Other (see comment). Avoid or Use Alternate Drug. Comment: Avoid use of metoclopramide intranasal or interacting drug, depending on importance of drug to patient. - metoprolol
paroxetine will increase the level or effect of metoprolol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- mexiletine
paroxetine will increase the level or effect of mexiletine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- milnacipran
milnacipran and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug.
- morphine
paroxetine will increase the level or effect of morphine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
morphine, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug. - nebivolol
paroxetine will increase the level or effect of nebivolol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- nefazodone
nefazodone and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug.
- netupitant/palonosetron
netupitant/palonosetron, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug.
- nortriptyline
paroxetine will increase the level or effect of nortriptyline by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
paroxetine and nortriptyline both increase serotonin levels. Avoid or Use Alternate Drug. - olanzapine
olanzapine and paroxetine both increase QTc interval. Avoid or Use Alternate Drug.
- olopatadine intranasal
paroxetine and olopatadine intranasal both increase sedation. Avoid or Use Alternate Drug. Coadministration increases risk of CNS depression, which can lead to additive impairment of psychomotor performance and cause daytime impairment.
- ondansetron
ondansetron, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug.
- oxycodone
paroxetine will increase the level or effect of oxycodone by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- oxymorphone
paroxetine will increase the level or effect of oxymorphone by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- ozanimod
ozanimod increases toxicity of paroxetine by sympathetic (adrenergic) effects, including increased blood pressure and heart rate. Avoid or Use Alternate Drug. Because the active metabolite of ozanimod inhibits MAO-B in vitro, there is a potential for serious adverse reactions, including hypertensive crisis. Therefore, coadministration of ozanimod with drugs that can increase norepinephrine or serotonin is not recommended. Monitor for hypertension with concomitant use.
- palonosetron
palonosetron, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug.
- pentamidine
paroxetine and pentamidine both increase QTc interval. Avoid or Use Alternate Drug.
- perphenazine
paroxetine will increase the level or effect of perphenazine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
perphenazine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
perphenazine and paroxetine both increase QTc interval. Avoid or Use Alternate Drug. - phentermine
paroxetine, phentermine. Either increases toxicity of the other by Mechanism: unknown. Avoid or Use Alternate Drug. Risk of serotonin syndrome.
- procainamide
paroxetine and procainamide both increase QTc interval. Avoid or Use Alternate Drug.
- promethazine
paroxetine will increase the level or effect of promethazine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- propafenone
paroxetine will increase the level or effect of propafenone by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
propafenone will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug. Monitor heart rate and EKG in patients receiving concurrent paroxetine and propafenone. Doses may need to be reduced. - propranolol
paroxetine will increase the level or effect of propranolol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- protriptyline
paroxetine and protriptyline both increase serotonin levels. Avoid or Use Alternate Drug.
- quinidine
quinidine and paroxetine both increase QTc interval. Avoid or Use Alternate Drug.
- rasagiline
rasagiline and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug. Severe CNS toxicity associated with hyperpyrexia has been reported with the combined treatment of an antidepressant and rasagiline. Avoid combination within 14 days of MAOI use.
- remifentanil
remifentanil, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug.
- selegiline transdermal
selegiline transdermal and paroxetine both increase serotonin levels. Avoid or Use Alternate Drug.
- selinexor
selinexor, paroxetine. unspecified interaction mechanism. Avoid or Use Alternate Drug. Patients treated with selinexor may experience neurological toxicities. Avoid taking selinexor with other medications that may cause dizziness or confusion.
- sertraline
sertraline will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
paroxetine and sertraline both increase serotonin levels. Avoid or Use Alternate Drug. - sotalol
paroxetine and sotalol both increase QTc interval. Avoid or Use Alternate Drug.
- St John's Wort
paroxetine and St John's Wort both increase serotonin levels. Avoid or Use Alternate Drug.
- sufentanil
sufentanil, paroxetine. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug.
- tedizolid
tedizolid, paroxetine. Either increases effects of the other by Mechanism: pharmacodynamic synergism. Avoid or Use Alternate Drug. both increase serotonin levels; increased risk of serotonin syndrome.
- tetrabenazine
tetrabenazine and paroxetine both increase QTc interval. Avoid or Use Alternate Drug.
- thioridazine
paroxetine will increase the level or effect of thioridazine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
thioridazine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
thioridazine and paroxetine both increase QTc interval. Avoid or Use Alternate Drug. - timolol
paroxetine will increase the level or effect of timolol by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- tipranavir
tipranavir will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- tolterodine
paroxetine will increase the level or effect of tolterodine by affecting hepatic enzyme CYP2D6 metabolism. Avoid or Use Alternate Drug.
- trazodone
paroxetine and trazodone both increase serotonin levels. Avoid or Use Alternate Drug.
- trimipramine
paroxetine and trimipramine both increase serotonin levels. Avoid or Use Alternate Drug.
- venlafaxine
paroxetine and venlafaxine both increase serotonin levels. Avoid or Use Alternate Drug.
- vilazodone
paroxetine, vilazodone. Either increases toxicity of the other by serotonin levels. Avoid or Use Alternate Drug. Concomitant therapy should be discontinued immediately if signs or symptoms of serotonin syndrome emerge and supportive symptomatic treatment should be initiated. .
- vortioxetine
paroxetine, vortioxetine. Either increases effects of the other by serotonin levels. Avoid or Use Alternate Drug.
- zuranolone
paroxetine, zuranolone. Either increases effects of the other by pharmacodynamic synergism. Avoid or Use Alternate Drug. Coadministration of zuranolone with other CNS depressants may increase impairment of psychomotor performance or CNS depressant effects. If unavoidable, consider dose reduction. .
Monitor Closely (244)
- 5-HTP
paroxetine and 5-HTP both increase serotonin levels. Modify Therapy/Monitor Closely.
- abiraterone
abiraterone increases levels of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Avoid coadministration of abiraterone with substrates of CYP2D6. If alternative therapy cannot be used, exercise caution and consider a dose reduction of the CYP2D6 substrate.
- aceclofenac
paroxetine, aceclofenac. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- acemetacin
paroxetine, acemetacin. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- alfuzosin
paroxetine and alfuzosin both increase QTc interval. Use Caution/Monitor.
- almotriptan
almotriptan and paroxetine both increase serotonin levels. Modify Therapy/Monitor Closely.
- American ginseng
American ginseng increases toxicity of paroxetine by pharmacodynamic synergism. Use Caution/Monitor. May have anticoagulant/antiplatelet effects.
- amifampridine
paroxetine increases toxicity of amifampridine by Other (see comment). Modify Therapy/Monitor Closely. Comment: Amifampridine can cause seizures. Coadministration with drugs that lower seizure threshold may increase this risk.
- amiodarone
amiodarone will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- amitriptyline
amitriptyline and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- amoxapine
amoxapine and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- anagrelide
anagrelide and paroxetine both increase QTc interval. Use Caution/Monitor.
- apixaban
paroxetine increases effects of apixaban by anticoagulation. Use Caution/Monitor. SSRIs may inhibit platelet aggregation, thus increase bleeding risk when coadministered with anticoagulants.
- aripiprazole
paroxetine, aripiprazole. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction).
- artemether/lumefantrine
artemether/lumefantrine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
artemether/lumefantrine and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely. - asenapine
asenapine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
paroxetine, asenapine. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction). - aspirin
paroxetine, aspirin. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- aspirin rectal
paroxetine, aspirin rectal. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- aspirin/citric acid/sodium bicarbonate
paroxetine, aspirin/citric acid/sodium bicarbonate. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- atogepant
paroxetine will increase the level or effect of atogepant by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- atomoxetine
paroxetine will increase the level or effect of atomoxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Reduced initial doses of atomoxetine are recommended with strong CYP2D6 inhibitors.
- avapritinib
paroxetine will increase the level or effect of avapritinib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- axitinib
paroxetine increases levels of axitinib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- benzhydrocodone/acetaminophen
benzhydrocodone/acetaminophen, paroxetine. Either increases effects of the other by serotonin levels. Use Caution/Monitor. Coadministration of drugs that affect the serotonergic neurotransmitter system may result in serotonin syndrome. If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation and dose adjustment.
- betrixaban
paroxetine, betrixaban. Either increases levels of the other by anticoagulation. Use Caution/Monitor. SSRIs may inhibit platelet aggregation, thus increase bleeding risk when coadministered with anticoagulants.
- brexpiprazole
paroxetine will increase the level or effect of brexpiprazole by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. Administer half of the usual brexpiprazole dose when coadministered with strong CYP2D6 inhibitors. If also administered with a strong/moderate CYP3A4 inhibitor, administer a quarter of brexpiprazole dose. NOTE: In MDD clinical trials, brexpiprazole dosage was not adjusted for strong CYP2D6 inhibitors (eg, paroxetine, fluoxetine); thus, CYP considerations are already factored into general dosing recommendations and brexpiprazole may be administered without dosage adjustment in patients with MDD.
- buprenorphine
buprenorphine and paroxetine both increase QTc interval. Use Caution/Monitor.
- buprenorphine buccal
buprenorphine buccal and paroxetine both increase QTc interval. Use Caution/Monitor.
- buprenorphine subdermal implant
paroxetine, buprenorphine subdermal implant. Either increases toxicity of the other by serotonin levels. Use Caution/Monitor. Concomitant use could result in life-threatening serotonin syndrome. If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation, and during dose adjustment of the serotonergic drug. Discontinue buprenorphine if serotonin syndrome is suspected.
- buprenorphine transdermal
buprenorphine transdermal and paroxetine both increase QTc interval. Use Caution/Monitor.
- buprenorphine, long-acting injection
paroxetine, buprenorphine, long-acting injection. Either increases toxicity of the other by serotonin levels. Use Caution/Monitor. Concomitant use could result in life-threatening serotonin syndrome. If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation, and during dose adjustment of the serotonergic drug. Discontinue buprenorphine if serotonin syndrome is suspected.
buprenorphine, long-acting injection and paroxetine both increase QTc interval. Use Caution/Monitor. - cariprazine
paroxetine, cariprazine. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction).
- celecoxib
paroxetine, celecoxib. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- cenobamate
cenobamate, paroxetine. Either increases effects of the other by sedation. Use Caution/Monitor.
- chlorpromazine
chlorpromazine and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- choline magnesium trisalicylate
paroxetine, choline magnesium trisalicylate. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- cimetidine
cimetidine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- clarithromycin
clarithromycin and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- clobazam
clobazam will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Lower doses of drugs metabolized by CYP2D6 may be required when used concomitantly.
- clomipramine
clomipramine and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- clonidine
clonidine, paroxetine. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Coadministration enhances CNS depressant effects.
- clopidogrel
paroxetine increases effects of clopidogrel by pharmacodynamic synergism. Use Caution/Monitor. SSRIs affect platelet activation; coadministration of SSRIs with clopidogrel may increase the risk of bleeding.
- clozapine
paroxetine increases levels of clozapine by decreasing metabolism. Use Caution/Monitor. Plasma levels of clozapine may be increased, resulting in increased pharmacologic and toxic effects. Adjust clozapine dose as needed when initiating or discontinuing certain SSRIs. .
paroxetine, clozapine. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction). - cobicistat
cobicistat will increase the level or effect of paroxetine by Other (see comment). Use Caution/Monitor. Carefully titrate dose of the antidepressant to the desired effect, including using the lowest feasible initial or maintenance dose, and monitor its response during coadministration with SSRIs and cobicistat.
- cocaine topical
paroxetine and cocaine topical both increase serotonin levels. Modify Therapy/Monitor Closely.
- codeine
paroxetine will decrease the level or effect of codeine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Prevents conversion of codeine to its active metabolite morphine.
- cyproheptadine
cyproheptadine decreases effects of paroxetine by pharmacodynamic antagonism. Use Caution/Monitor. Cyproheptadine may diminish the serotonergic effect of SSRIs.
- daridorexant
paroxetine and daridorexant both increase sedation. Modify Therapy/Monitor Closely. Coadministration increases risk of CNS depression, which can lead to additive impairment of psychomotor performance and cause daytime impairment.
- darunavir
darunavir decreases levels of paroxetine by Mechanism: unspecified interaction mechanism. Use Caution/Monitor. Carefully titrate SSRI dose based on clinical assessment of antidepressant response.
darunavir will increase the level or effect of paroxetine by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Coadministration with SSRIs, TCAs, or trazodone may require dose titration of antidepressant to desired effect (eg, using the lowest feasible initial or maintenance dose). Monitor for antidepressant response. - dasatinib
dasatinib and paroxetine both increase QTc interval. Use Caution/Monitor.
- defibrotide
defibrotide increases effects of paroxetine by Other (see comment). Use Caution/Monitor. Comment: Defibrotide may enhance effects of platelet inhibitors.
- desipramine
desipramine and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- desvenlafaxine
desvenlafaxine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Desvenlafaxine inhibits CYP2D6; with higher desvenlafaxine doses (ie, 400 mg) decrease the CYP2D6 substrate dose by up to 50%; no dosage adjustment needed with desvenlafaxine doses <100 mg
- deutetrabenazine
paroxetine will increase the level or effect of deutetrabenazine by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. Strong CYP2D6 inhibitors increase the systemic exposure to the active dihydro-metabolites of deutetrabenazine by approximately 3-fold. Do not exceed 18 mg/dose and 36 mg/day of deutetrabenazine if coadministered with strong CYP2D6 inhibitors.
deutetrabenazine and paroxetine both increase QTc interval. Use Caution/Monitor. At the maximum recommended dose, deutetrabenazine does not prolong QT interval to a clinically relevant extent. Certain circumstances may increase risk of torsade de pointes and/or sudden death in association with drugs that prolong the QTc interval (eg, bradycardia, hypokalemia or hypomagnesemia, coadministration with other drugs that prolong QTc interval, presence of congenital QT prolongation). - dexfenfluramine
paroxetine will increase the level or effect of dexfenfluramine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
paroxetine and dexfenfluramine both increase serotonin levels. Modify Therapy/Monitor Closely. - dextroamphetamine
paroxetine will increase the level or effect of dextroamphetamine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
paroxetine and dextroamphetamine both increase serotonin levels. Modify Therapy/Monitor Closely. - dextroamphetamine transdermal
paroxetine, dextroamphetamine transdermal. Either increases effects of the other by serotonin levels. Modify Therapy/Monitor Closely. Initiate with lower doses and monitor for signs and symptoms of serotonin syndrome, particularly during initiation or dosage increase. If serotonin syndrome occurs, discontinue dextroamphetamine transdermal and concomitant serotonergic drug(s).
paroxetine will increase the level or effect of dextroamphetamine transdermal by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. Initiate with lower doses and monitor patients for signs and symptoms of serotonin syndrome, particularly during dextroamphetamine initiation and after a dosage increase. If serotonin syndrome occurs, discontinue dextroamphetamine transdermal and CYP2D6 inhibitor. - diazepam intranasal
diazepam intranasal, paroxetine. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Coadministration may potentiate the CNS-depressant effects of each drug.
- dichlorphenamide
dichlorphenamide and paroxetine both decrease serum potassium. Use Caution/Monitor.
- diclofenac
paroxetine, diclofenac. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- difelikefalin
difelikefalin and paroxetine both increase sedation. Use Caution/Monitor.
- diflunisal
paroxetine, diflunisal. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- dihydroergotamine
paroxetine and dihydroergotamine both increase serotonin levels. Modify Therapy/Monitor Closely.
- dihydroergotamine intranasal
paroxetine and dihydroergotamine intranasal both increase serotonin levels. Modify Therapy/Monitor Closely.
- dofetilide
dofetilide and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- dolasetron
dolasetron and paroxetine both increase QTc interval. Use Caution/Monitor.
- donepezil
paroxetine will increase the level or effect of donepezil by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
donepezil and paroxetine both increase QTc interval. Use Caution/Monitor. - doxepin
doxepin and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- dronedarone
dronedarone will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
dronedarone and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely. - droperidol
droperidol and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- edoxaban
paroxetine increases effects of edoxaban by anticoagulation. Use Caution/Monitor. SSRIs may inhibit platelet aggregation, thus increase bleeding risk when coadministered with anticoagulants.
- eletriptan
eletriptan and paroxetine both increase serotonin levels. Modify Therapy/Monitor Closely.
- eliglustat
eliglustat increases levels of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. Monitor therapeutic drug concentrations, as indicated, or consider reducing the dosage of the concomitant drug and titrate to clinical effect.
- eluxadoline
paroxetine increases levels of eluxadoline by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. As a precautionary measure due to incomplete information on the metabolism of eluxadoline, use caution when coadministered with strong CYP2D6 inhibitors.
- elvitegravir/cobicistat/emtricitabine/tenofovir DF
elvitegravir/cobicistat/emtricitabine/tenofovir DF increases levels of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. Cobicistat is a CYP2D6 inhibitor; caution with CYP2D6 substrates for which elevated plasma concentrations are associated with serious and/or life-threatening events.
- encainide
paroxetine will increase the level or effect of encainide by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- epinephrine
epinephrine and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- epinephrine racemic
epinephrine racemic and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- ergotamine
paroxetine and ergotamine both increase serotonin levels. Modify Therapy/Monitor Closely.
- erythromycin base
erythromycin base and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- erythromycin ethylsuccinate
erythromycin ethylsuccinate and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- erythromycin lactobionate
erythromycin lactobionate and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- erythromycin stearate
erythromycin stearate and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- etodolac
paroxetine, etodolac. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- fedratinib
fedratinib will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Adjust dose of drugs that are CYP2D6 substrates as necessary.
- fenbufen
paroxetine, fenbufen. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- fenfluramine
paroxetine and fenfluramine both increase serotonin levels. Modify Therapy/Monitor Closely.
fenfluramine, paroxetine. Either increases effects of the other by serotonin levels. Use Caution/Monitor. Coadministration with drugs that increase serotoninergic effects may increase the risk of serotonin syndrome. - fenoprofen
paroxetine, fenoprofen. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- finerenone
paroxetine will increase the level or effect of finerenone by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Monitor serum potassium during initiation and dosage adjustment of either finererone or weak CYP3A4 inhibitors. Adjust finererone dosage as needed.
- fish oil triglycerides
fish oil triglycerides will increase the level or effect of paroxetine by anticoagulation. Use Caution/Monitor. Prolonged bleeding reported in patients taking antiplatelet agents or anticoagulants and oral omega-3 fatty acids. Periodically monitor bleeding time in patients receiving fish oil triglycerides and concomitant antiplatelet agents or anticoagulants.
- flecainide
flecainide and paroxetine both increase QTc interval. Use Caution/Monitor.
- flibanserin
paroxetine will increase the level or effect of flibanserin by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Increased flibanserin adverse effects may occur if coadministered with multiple weak CYP3A4 inhibitors.
- fluconazole
fluconazole and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- fluoxetine
fluoxetine and paroxetine both increase QTc interval. Use Caution/Monitor.
- fluphenazine
paroxetine, fluphenazine. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction).
- flurbiprofen
paroxetine, flurbiprofen. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- fluvoxamine
fluvoxamine and paroxetine both increase QTc interval. Use Caution/Monitor.
- fondaparinux
paroxetine increases effects of fondaparinux by anticoagulation. Use Caution/Monitor. SSRIs may inhibit platelet aggregation, thus increase bleeding risk when coadministered with anticoagulants.
- formoterol
formoterol and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- fosamprenavir
fosamprenavir will decrease the level or effect of paroxetine by increasing elimination. Use Caution/Monitor. Monitor response to paroxetine therapy closely
- foscarnet
foscarnet and paroxetine both increase QTc interval. Use Caution/Monitor.
- frovatriptan
frovatriptan and paroxetine both increase serotonin levels. Modify Therapy/Monitor Closely.
- gabapentin
gabapentin, paroxetine. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Coadministration of CNS depressants can result in serious, life-threatening, and fatal respiratory depression. Use lowest dose possible and monitor for respiratory depression and sedation.
- gabapentin enacarbil
gabapentin enacarbil, paroxetine. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Coadministration of CNS depressants can result in serious, life-threatening, and fatal respiratory depression. Use lowest dose possible and monitor for respiratory depression and sedation.
- galantamine
paroxetine will increase the level or effect of galantamine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- ganaxolone
paroxetine and ganaxolone both increase sedation. Use Caution/Monitor.
- gepirone
gepirone and paroxetine both increase serotonin levels. Use Caution/Monitor. Monitor for symptoms of serotonin syndrome when gepirone is used gepirone with other drugs that may affect the serotonergic neurotransmitter systems. If serotonin syndrome occurs, consider discontinue gepirone and/or concomitant serotonergic drug.
- givinostat
paroxetine and givinostat both increase QTc interval. Use Caution/Monitor. If coadministered, obtain ECGs when initiating, during concomitant use, and as clinically indicated. Withhold if QTc interval >500 ms or a change from baseline >60 ms.
- green tea
green tea, paroxetine. Other (see comment). Use Caution/Monitor. Comment: Combination may increase risk of bleeding.
- haloperidol
haloperidol will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
haloperidol and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
paroxetine, haloperidol. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction). - hydrocodone
paroxetine will increase the level or effect of hydrocodone by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Hydromorphone (<3% of the circulating parent hydrocodone) is mainly formed by CYP2D6 mediated O-demethylation of hydrocodone. Hydromorphone may contribute to the total analgesic effect of hydrocodone.
hydrocodone, paroxetine. Either increases effects of the other by serotonin levels. Use Caution/Monitor. Coadministration of drugs that affect the serotonergic neurotransmitter system may result in serotonin syndrome. If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation and dose adjustment. - hydroxyzine
hydroxyzine and paroxetine both increase QTc interval. Use Caution/Monitor.
- ibrutinib
ibrutinib will increase the level or effect of paroxetine by anticoagulation. Use Caution/Monitor. Ibrutinib may increase the risk of hemorrhage in patients receiving antiplatelet or anticoagulant therapies and monitor for signs of bleeding.
- ibuprofen
paroxetine, ibuprofen. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- ibuprofen IV
paroxetine, ibuprofen IV. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- icosapent
icosapent, paroxetine. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Icosapent may prolong bleeding time. Periodically monitor if coadministered with other drugs that affect bleeding.
- iloperidone
iloperidone and paroxetine both increase QTc interval. Use Caution/Monitor.
paroxetine, iloperidone. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction). - imatinib
imatinib will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- imipramine
imipramine and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- indomethacin
paroxetine, indomethacin. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- ioflupane I 123
paroxetine decreases effects of ioflupane I 123 by receptor binding competition. Use Caution/Monitor. Drugs that bind to dopamine transporter receptor with high affinity may interfere with the image following ioflupane I 123 administration.
- isavuconazonium sulfate
paroxetine will increase the level or effect of isavuconazonium sulfate by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- isoniazid
paroxetine and isoniazid both increase serotonin levels. Modify Therapy/Monitor Closely.
- itraconazole
itraconazole and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- ivacaftor
paroxetine increases levels of ivacaftor by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Monitor when coadministered with weak CYP3A4 inhibitors .
- ketoconazole
ketoconazole and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- ketoprofen
paroxetine, ketoprofen. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- ketorolac
paroxetine, ketorolac. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- ketorolac intranasal
paroxetine, ketorolac intranasal. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- L-tryptophan
paroxetine and L-tryptophan both increase serotonin levels. Modify Therapy/Monitor Closely.
- lamotrigine
lamotrigine increases toxicity of paroxetine by unspecified interaction mechanism. Modify Therapy/Monitor Closely. CNS depressants may increase the toxic effects of selective serotonin reuptake inhibitors; psychomotor impairment may be enhanced.
- lapatinib
lapatinib and paroxetine both increase QTc interval. Use Caution/Monitor.
- lasmiditan
lasmiditan, paroxetine. Either increases effects of the other by sedation. Use Caution/Monitor. Coadministration of lasmiditan and other CNS depressant drugs, including alcohol have not been evaluated in clinical studies. Lasmiditan may cause sedation, as well as other cognitive and/or neuropsychiatric adverse reactions.
paroxetine increases effects of lasmiditan by serotonin levels. Use Caution/Monitor. Coadministration may increase risk of serotonin syndrome. - lemborexant
paroxetine will increase the level or effect of lemborexant by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Modify Therapy/Monitor Closely. Lower nightly dose of lemborexant recommended if coadministered with weak CYP3A4 inhibitors. See drug monograph for specific dosage modification.
lemborexant, paroxetine. Either increases effects of the other by sedation. Modify Therapy/Monitor Closely. Dosage adjustment may be necessary if lemborexant is coadministered with other CNS depressants because of potentially additive effects. - levofloxacin
levofloxacin and paroxetine both increase QTc interval. Use Caution/Monitor.
- levoketoconazole
levoketoconazole and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- lisdexamfetamine
paroxetine, lisdexamfetamine. Either increases effects of the other by serotonin levels. Use Caution/Monitor. Initiate with lower doses and monitor for signs and symptoms of serotonin syndrome, particularly during initiation or dosage increase. If serotonin syndrome occurs, discontinue along with concomitant serotonergic drug(s).
- lithium
paroxetine and lithium both increase serotonin levels. Modify Therapy/Monitor Closely.
lithium and paroxetine both increase QTc interval. Use Caution/Monitor. - lofepramine
lofepramine and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- lofexidine
paroxetine will increase the level or effect of lofexidine by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. Concomitant use of lofexidine with strong CYP2D6 inhibitors may increase lofexidine plasma levels. Monitor for symptoms of orthostasis and bradycardia if coadministered with a CYP2D6 inhibitor. Consider lofexidine dose reduction.
- lomitapide
paroxetine increases levels of lomitapide by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Lomitapide dose should not exceed 30 mg/day.
- loratadine
paroxetine will increase the level or effect of loratadine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- lorcaserin
lorcaserin will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- lornoxicam
paroxetine, lornoxicam. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- loxapine
paroxetine, loxapine. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction).
- loxapine inhaled
paroxetine, loxapine inhaled. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction).
- lsd
paroxetine and lsd both increase serotonin levels. Modify Therapy/Monitor Closely.
- lumefantrine
lumefantrine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
lumefantrine and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely. - lurasidone
lurasidone, paroxetine. Either increases toxicity of the other by Other (see comment). Use Caution/Monitor. Comment: Potential for increased CNS depressant effects when used concurrently; monitor for increased adverse effects and toxicity.
paroxetine, lurasidone. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction). - maprotiline
maprotiline and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- mavacamten
paroxetine will increase the level or effect of mavacamten by affecting hepatic enzyme CYP2C19 metabolism. Modify Therapy/Monitor Closely. Inititiation of weak CYP2C19 inhibitors may require decreased mavacamten dose.
- meclofenamate
paroxetine, meclofenamate. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- mefenamic acid
paroxetine, mefenamic acid. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- meloxicam
paroxetine, meloxicam. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- metformin
paroxetine increases effects of metformin by pharmacodynamic synergism. Use Caution/Monitor.
- methadone
methadone and paroxetine both increase QTc interval. Use Caution/Monitor.
- methylphenidate transdermal
methylphenidate transdermal will increase the level or effect of paroxetine by decreasing metabolism. Modify Therapy/Monitor Closely. Consider decreasing the dose of these drugs when given coadministered with methylphenidate. Monitor for drug toxiticities when initiating or discontinuing methylphenidate.
- midazolam intranasal
paroxetine will increase the level or effect of midazolam intranasal by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor. Coadministration of mild CYP3A4 inhibitors with midazolam intranasal may cause higher midazolam systemic exposure, which may prolong sedation.
midazolam intranasal, paroxetine. Either increases toxicity of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Concomitant use of barbiturates, alcohol, or other CNS depressants may increase the risk of hypoventilation, airway obstruction, desaturation, or apnea and may contribute to profound and/or prolonged drug effect. - mipomersen
mipomersen, paroxetine. Either increases toxicity of the other by Other (see comment). Use Caution/Monitor. Comment: Both drugs have potential to increase hepatic enzymes; monitor LFTs.
- mirabegron
mirabegron will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- mirtazapine
paroxetine and mirtazapine both increase serotonin levels. Modify Therapy/Monitor Closely.
mirtazapine and paroxetine both increase QTc interval. Use Caution/Monitor. - molindone
paroxetine, molindone. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction).
- morphine
paroxetine and morphine both increase serotonin levels. Modify Therapy/Monitor Closely.
- moxifloxacin
moxifloxacin and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
paroxetine and moxifloxacin both increase QTc interval. Modify Therapy/Monitor Closely. - nabumetone
paroxetine, nabumetone. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- naproxen
paroxetine, naproxen. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- naratriptan
naratriptan and paroxetine both increase serotonin levels. Modify Therapy/Monitor Closely.
- nilotinib
nilotinib and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- nortriptyline
nortriptyline and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- octreotide
octreotide and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- octreotide (Antidote)
octreotide (Antidote) and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- ofloxacin
ofloxacin and paroxetine both increase QTc interval. Use Caution/Monitor.
- olanzapine
paroxetine, olanzapine. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction).
- olanzapine/samidorphan
paroxetine, olanzapine/samidorphan. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Coadministration of diazepam, alcohol, or other CNS acting drugs may potentiate orthostatic hypotension observed with olanzapine. Additive sedation may also occur.
- oliceridine
paroxetine will increase the level or effect of oliceridine by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. If concomitant use is necessary, may require less frequent oliceridine dosing. Closely monitor for respiratory depression and sedation and titrate subsequent doses accordingly. If inhibitor is discontinued, consider increase oliceridine dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal.
paroxetine, oliceridine. Either increases toxicity of the other by serotonin levels. Modify Therapy/Monitor Closely. - oxaprozin
paroxetine, oxaprozin. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- oxycodone
oxycodone increases effects of paroxetine by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Opioids may enhance the serotonergic effects of SSRIs and increase risk for serotonergic syndrome.
- paliperidone
paliperidone and paroxetine both increase QTc interval. Use Caution/Monitor.
paroxetine, paliperidone. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction). - panax ginseng
panax ginseng decreases toxicity of paroxetine by pharmacodynamic synergism. Use Caution/Monitor. May have anticoagulant/antiplatelet effects.
- parecoxib
paroxetine, parecoxib. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- peginterferon alfa 2b
peginterferon alfa 2b, paroxetine. Other (see comment). Use Caution/Monitor. Comment: When patients are administered peginterferon alpha-2b with CYP2D6 substrates, the therapeutic effect of these drugs may be altered. Peginterferon alpha-2b may increase or decrease levels of CYP2D6 substrate.
- pentazocine
paroxetine and pentazocine both increase serotonin levels. Modify Therapy/Monitor Closely.
- perhexiline
paroxetine will increase the level or effect of perhexiline by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- perphenazine
paroxetine, perphenazine. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction).
- pimavanserin
paroxetine, pimavanserin. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction).
- pimozide
paroxetine, pimozide. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction).
- piroxicam
paroxetine, piroxicam. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- pitolisant
paroxetine and pitolisant both increase affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. If coadministered with strong CYP2D6 inhibitors, initiate pitolisant at 8.9 mg/day and increase after 7 days to maximum of 17.8 mg/day. For patients currently taking pitolisant, reduce pitolisant dose by half upon initiating strong CYP2D6 inhibitors.
- posaconazole
paroxetine and posaconazole both increase QTc interval. Use Caution/Monitor.
- pregabalin
pregabalin, paroxetine. Either increases effects of the other by pharmacodynamic synergism. Modify Therapy/Monitor Closely. Coadministration of CNS depressants can result in serious, life-threatening, and fatal respiratory depression. Use lowest dose possible and monitor for respiratory depression and sedation.
- prochlorperazine
paroxetine will increase the level or effect of prochlorperazine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
prochlorperazine and paroxetine both increase QTc interval. Use Caution/Monitor. - promazine
paroxetine will increase the level or effect of promazine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
promazine and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely. - promethazine
promethazine and paroxetine both increase QTc interval. Use Caution/Monitor.
- protriptyline
protriptyline and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- quetiapine
paroxetine, quetiapine. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction).
- quinidine
quinidine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Monitor patients for signs of paroxetine toxicity. Paroxetine doses may need to be reduced.
- ranolazine
paroxetine and ranolazine both increase QTc interval. Use Caution/Monitor.
- remimazolam
remimazolam, paroxetine. Either increases toxicity of the other by sedation. Modify Therapy/Monitor Closely. Coadministration may result in profound sedation, respiratory depression, coma, and/or death. Continuously monitor vital signs during sedation and recovery period if coadministered. Carefully titrate remimazolam dose if administered with opioid analgesics and/or sedative/hypnotics.
- risperidone
paroxetine will increase the level or effect of risperidone by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
paroxetine and risperidone both increase QTc interval. Use Caution/Monitor.
paroxetine increases levels of risperidone by decreasing metabolism. Use Caution/Monitor.
paroxetine, risperidone. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction). - ritonavir
ritonavir will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- rivaroxaban
paroxetine increases effects of rivaroxaban by pharmacodynamic synergism. Use Caution/Monitor. Combination may increase risk of bleeding.
- rizatriptan
rizatriptan and paroxetine both increase serotonin levels. Modify Therapy/Monitor Closely.
- rolapitant
rolapitant will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Rolapitant may increase plasma concentrations of CYP2D6 substrates for at least 28 days following rolapitant administration.
- safinamide
paroxetine, safinamide. Either increases toxicity of the other by serotonin levels. Use Caution/Monitor. Monitor patients for symptoms of serotonin syndrome if SSRIs are coadministered with safinamide.
- salicylates (non-asa)
paroxetine, salicylates (non-asa). Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- salsalate
paroxetine, salsalate. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- SAMe
paroxetine and SAMe both increase serotonin levels. Modify Therapy/Monitor Closely.
- sertraline
sertraline and paroxetine both increase QTc interval. Use Caution/Monitor.
- Siberian ginseng
Siberian ginseng increases toxicity of paroxetine by pharmacodynamic synergism. Use Caution/Monitor. May have anticoagulant/antiplatelet effects.
- sodium sulfate/?magnesium sulfate/potassium chloride
sodium sulfate/?magnesium sulfate/potassium chloride increases effects of paroxetine by unknown mechanism. Use Caution/Monitor. Closely monitor for evidence of seizures when using bowel preps together with drugs that lower the seizure threshold.
- sodium sulfate/potassium chloride/magnesium sulfate/polyethylene glycol
paroxetine, sodium sulfate/potassium chloride/magnesium sulfate/polyethylene glycol. Other (see comment). Use Caution/Monitor. Comment: Caution when bowel preps are used with drugs that cause SIADH or NSAIDs; increased risk for water retention or electrolyte imbalance.
- sodium sulfate/potassium sulfate/magnesium sulfate
sodium sulfate/potassium sulfate/magnesium sulfate increases effects of paroxetine by unknown mechanism. Use Caution/Monitor. Closely monitor for evidence of seizures when using bowel preps together with drugs that lower the seizure threshold.
- sufentanil SL
sufentanil SL, paroxetine. Either increases effects of the other by serotonin levels. Use Caution/Monitor. Coadministration of drugs that affect the serotonergic neurotransmitter system may result in serotonin syndrome. If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation and dose adjustment.
- sulfamethoxazole
sulfamethoxazole and paroxetine both increase QTc interval. Use Caution/Monitor.
- sulfasalazine
paroxetine, sulfasalazine. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- sulindac
paroxetine, sulindac. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- sumatriptan
sumatriptan and paroxetine both increase serotonin levels. Modify Therapy/Monitor Closely.
- sumatriptan intranasal
sumatriptan intranasal and paroxetine both increase serotonin levels. Modify Therapy/Monitor Closely.
- tamoxifen
paroxetine decreases effects of tamoxifen by decreasing metabolism. Use Caution/Monitor. Inhibition of CYP2D6 metabolism to tamoxifen's active metabolite, endoxifen.
- tamsulosin
paroxetine increases levels of tamsulosin by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
- tapentadol
paroxetine and tapentadol both increase serotonin levels. Modify Therapy/Monitor Closely.
- tazemetostat
paroxetine will increase the level or effect of tazemetostat by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- telavancin
paroxetine and telavancin both increase QTc interval. Use Caution/Monitor.
- terbinafine
terbinafine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. Assess need to reduce dose of CYP2D6-metabolized drug.
- tetrabenazine
paroxetine increases effects of tetrabenazine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Decrease tetrabenazine dose by 50% when coadministered with strong CYP2D6 inhibitors.
- thiothixene
paroxetine, thiothixene. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction).
- tinidazole
paroxetine will increase the level or effect of tinidazole by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Use Caution/Monitor.
- tolfenamic acid
paroxetine, tolfenamic acid. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- tolmetin
paroxetine, tolmetin. Either increases toxicity of the other by pharmacodynamic synergism. Use Caution/Monitor. Increased risk of upper GI bleeding. SSRIs inhib. serotonin uptake by platelets.
- tramadol
paroxetine decreases effects of tramadol by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor. Decreased conversion of tramadol to active metabolite.
paroxetine and tramadol both increase serotonin levels. Modify Therapy/Monitor Closely. - trazodone
trazodone and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- trifluoperazine
paroxetine will increase the level or effect of trifluoperazine by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
trifluoperazine and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
paroxetine, trifluoperazine. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction). - trimethoprim
paroxetine and trimethoprim both increase QTc interval. Use Caution/Monitor.
- trimipramine
trimipramine and paroxetine both increase QTc interval. Modify Therapy/Monitor Closely.
- tropisetron
paroxetine will increase the level or effect of tropisetron by affecting hepatic enzyme CYP2D6 metabolism. Use Caution/Monitor.
paroxetine and tropisetron both increase QTc interval. Use Caution/Monitor. - valbenazine
paroxetine will increase the level or effect of valbenazine by affecting hepatic enzyme CYP2D6 metabolism. Modify Therapy/Monitor Closely. Consider reducing valbenazine dose based on tolerability if coadministered with a strong CYP2D6 inhibitor.
valbenazine and paroxetine both increase QTc interval. Use Caution/Monitor. - valerian
valerian and paroxetine both increase sedation. Use Caution/Monitor.
- venlafaxine
paroxetine and venlafaxine both increase QTc interval. Use Caution/Monitor.
- vorapaxar
paroxetine, vorapaxar. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Additive antiplatelet effect may occur; SSRIs and SNRIs may cause platelet serotonin depletion .
- voriconazole
paroxetine and voriconazole both increase QTc interval. Use Caution/Monitor.
- warfarin
paroxetine, warfarin. Either increases effects of the other by pharmacodynamic synergism. Use Caution/Monitor. Serotonin release by platelets plays an important role in hemostasis. SSRIs and SNRIs may increase anticoagulation effect of warfarin. .
- zanubrutinib
paroxetine, zanubrutinib. Either increases effects of the other by anticoagulation. Modify Therapy/Monitor Closely. Zanubrutinib-induced cytopenias increases risk of hemorrhage. Coadministration of zanubritinib with antiplatelets or anticoagulants may further increase this risk.
- ziprasidone
paroxetine and ziprasidone both increase QTc interval. Modify Therapy/Monitor Closely.
paroxetine, ziprasidone. unspecified interaction mechanism. Use Caution/Monitor. Serotonin modulators may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotics may enhance serotonergic effect of serotonin modulators, which may result in serotonin syndrome. Monitor for evidence of serotonin toxicity (eg, mental status changes, autonomic instability, and neuromuscular hyperactivity) or neuroleptic malignant syndrome (eg, hyperthermia, muscle rigidity, autonomic dysfunction). - zolmitriptan
zolmitriptan and paroxetine both increase serotonin levels. Modify Therapy/Monitor Closely.
Minor (38)
- almotriptan
paroxetine, almotriptan. Mechanism: unknown. Minor/Significance Unknown. Risk of weakness, dyspnea, chest pain.
- aprepitant
aprepitant, paroxetine. Either decreases levels of the other by unspecified interaction mechanism. Minor/Significance Unknown.
- azithromycin
azithromycin and paroxetine both increase QTc interval. Minor/Significance Unknown.
- bumetanide
bumetanide, paroxetine. Mechanism: pharmacodynamic synergism. Minor/Significance Unknown. Possible additive hyponatremia.
- celandine
celandine decreases effects of paroxetine by pharmacodynamic antagonism. Minor/Significance Unknown. Based on animal studies.
- celecoxib
celecoxib will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- chloroquine
chloroquine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- darifenacin
darifenacin will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- dexmethylphenidate
dexmethylphenidate increases effects of paroxetine by decreasing metabolism. Minor/Significance Unknown.
- diphenhydramine
diphenhydramine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- duloxetine
duloxetine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- eletriptan
paroxetine, eletriptan. Mechanism: unknown. Minor/Significance Unknown. Risk of weakness, dyspnea, chest pain.
- ethacrynic acid
ethacrynic acid, paroxetine. Mechanism: pharmacodynamic synergism. Minor/Significance Unknown. Possible additive hyponatremia.
- fesoterodine
paroxetine will increase the level or effect of fesoterodine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- fosaprepitant
fosaprepitant, paroxetine. Either decreases levels of the other by unspecified interaction mechanism. Minor/Significance Unknown.
- frovatriptan
paroxetine, frovatriptan. Mechanism: unknown. Minor/Significance Unknown. Risk of weakness, dyspnea, chest pain.
- furosemide
furosemide, paroxetine. Mechanism: pharmacodynamic synergism. Minor/Significance Unknown. Possible additive hyponatremia.
- lithium
paroxetine, lithium. Mechanism: unknown. Minor/Significance Unknown. Risk of neurotoxicity.
- maraviroc
maraviroc will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- marijuana
marijuana will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- naratriptan
paroxetine, naratriptan. Mechanism: unknown. Minor/Significance Unknown. Risk of weakness, dyspnea, chest pain.
- nilotinib
nilotinib will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- oxycodone
paroxetine decreases effects of oxycodone by decreasing metabolism. Minor/Significance Unknown. Decreased conversion of oxycodone to active metabolite morphine.
- parecoxib
parecoxib will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- pazopanib
paroxetine and pazopanib both increase QTc interval. Minor/Significance Unknown.
- pleurisy root
pleurisy root decreases effects of paroxetine by unspecified interaction mechanism. Minor/Significance Unknown. Theoretical interaction.
- quinacrine
quinacrine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- ranolazine
ranolazine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- rizatriptan
paroxetine, rizatriptan. Mechanism: unknown. Minor/Significance Unknown. Risk of weakness, dyspnea, chest pain.
- ruxolitinib
paroxetine will increase the level or effect of ruxolitinib by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- ruxolitinib topical
paroxetine will increase the level or effect of ruxolitinib topical by affecting hepatic/intestinal enzyme CYP3A4 metabolism. Minor/Significance Unknown.
- serdexmethylphenidate/dexmethylphenidate
serdexmethylphenidate/dexmethylphenidate increases effects of paroxetine by decreasing metabolism. Minor/Significance Unknown.
- sumatriptan
paroxetine, sumatriptan. Mechanism: unknown. Minor/Significance Unknown. Risk of weakness, dyspnea, chest pain.
- sumatriptan intranasal
paroxetine, sumatriptan intranasal. Mechanism: unknown. Minor/Significance Unknown. Risk of weakness, dyspnea, chest pain.
- torsemide
torsemide, paroxetine. Mechanism: pharmacodynamic synergism. Minor/Significance Unknown. Possible additive hyponatremia.
- tramadol
paroxetine decreases effects of tramadol by decreasing metabolism. Minor/Significance Unknown. Decreased conversion of tramadol to active metabolite.
- venlafaxine
venlafaxine will increase the level or effect of paroxetine by affecting hepatic enzyme CYP2D6 metabolism. Minor/Significance Unknown.
- zolmitriptan
paroxetine, zolmitriptan. Mechanism: unknown. Minor/Significance Unknown. Risk of weakness, dyspnea, chest pain.
Adverse Effects
>10% (Based on 40 mg Dose)
Nausea (15-24%)
Insomnia (11-24%)
Dry mouth (9-18%)
Headache (17%)
Asthenia (10-15%)
Constipation (10-15%)
Diarrhea (9-12%)
Dizziness (6-14%)
Ejaculation disorder (10-15%)
Tremor (4-11%)
1-10% (Based on 40 mg Dose)
Anxiety (5-10%)
Blurred vision (5-10%)
Decreased appetite (5-10%)
Impotence (2-9%)
Nervousness (2-5%)
Paresthesia (2-5%)
Hypomania (0.3 to 2.2%)
Frequency Not Defined (Based on 40 mg Dose)
Hypertension
Tachycardia
Emotional lability
Pruritus
Weight gain
Arthralgia
Tinnitus
Vertigo
Angle clossure glaucoma
Serious
- Depression exacerbation
- Mania (rare)
- Serotonin syndrome
- Suicidal thoughts (rare)
- Suicide (rare)
- Seizure (rare)
- Toxic epidermal necrolysis
- Hyponatremia (rare)
- Bleeding, abnormal (rare)
- Acute hepatitis (rare)
- Stevens-Johnson Syndrome
- Bone fracture
- Akathisia
Warnings
Black Box Warnings
In short-term studies, antidepressants increased the risk of suicidal thinking and behavior in children, adolescents, and young adults (<24 years) taking antidepressants for major depressive disorders and other psychiatric illnesses
This increase was not seen in patients aged >24 years; a slight decrease in suicidal thinking was seen in adults >65 years
In children and young adults, risks must be weighed against the benefits of taking antidepressants
Patients should be monitored closely for changes in behavior, clinical worsening, and suicidal tendencies; this should be done during the initial 1-2 months of therapy and dosage adjustments
The patient’s family should communicate any abrupt changes in behavior to the healthcare provider
Worsening behavior and suicidal tendencies that are not part of the presenting symptoms may require discontinuation of therapy
This drug is not approved for use in pediatric patients
Contraindications
Hypersensitivity
Concomitant administration with pimozide or thioridazine
Coadministration with serotonergic drugs
- Concomitant use or within 14 days of MAOIs increases risk of serotonin syndrome
- Reactions to concomitant administration with MAOIs include tremor, myoclonus, diaphoresis, nausea, vomiting, flushing, dizziness, hyperthermia with features resembling neuroleptic malignant syndrome, seizures, rigidity, autonomic instability with possible rapid fluctuations of vital signs, and mental status changes that include extreme agitation progressing to delirium and coma
- Starting paroxetine in a patient who is being treated with linezolid or IV methylene blue is contraindicated because of an increased risk of serotonin syndrome
- If linezolid or IV methylene blue must be administered, discontinue SSRI immediately and monitor for CNS toxicity; may resume 24 hr after last linezolid or methylene blue dose, or after 2 weeks of monitoring (5 weeks for fluoxetine), whichever comes first
Cautions
Clinical worsening and suicidal ideation may occur despite medication in adolescents and young adults (18-24 years)
Use caution in patients with history of seizure or suicidal thought/behavior; discontinue therapy in patients who develop seizures
In patients with bipolar disorder, treating a depressive episode may precipitate a mixed/manic episode; prior to initiating treatment, screen patients for any personal or family history of bipolar disorder, mania, or hypomania
Adverse reactions after discontinuation of serotonergic antidepressants, particularly after abrupt discontinuation, include, nausea, sweating, dysphoric mood, irritability, agitation, dizziness, sensory disturbances (eg, paresthesia, such as electric shock sensations), tremor, anxiety, confusion, headache, lethargy, emotional lability, insomnia, hypomania, tinnitus, and seizures; a gradual reduction in dosage rather than abrupt cessation is recommended whenever possible
Life-threatening serotonin syndrome reported with SNRIs and SSRIs alone; also with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, amphetamines, and St. John’s Wort)
Risk of mydriasis; may trigger angle closure attack in patients with angle closure glaucoma with anatomically narrow angles without a patent iridectomy; avoid use in patients with untreated anatomically narrow angles
Conflicting evidence regarding use of SSRIs during pregnancy and increased risk of persistent pulmonary hypertension of the newborn (see Pregnancy)
Risk of complications such as feeding difficulties, irritability, and respiratory problems reported in neonates exposed to SNRIs/SSRIs late in third trimester
Risk of cardiovascular defects in infants whose mothers took drug during early pregnancy
Withdraw gradually
Use lower starting dose in renal impairment (CrCl <30 mL/min) or severe hepatic impairment
In patients with symptomatic hyponatremia, discontinue therapy and institute appropriate medical intervention; elderly patients, patients taking diuretics, and those who are volume-depleted may be at greater risk of developing hyponatremia with SSRIs
Inability to remain still due to feelings of agitation or restlessness reported; may occur within first few weeks of therapy
May impair platelet aggregation especially when used in combination with aspirin or NSAIDs; increases risk of bleeding in patients taking anticoagulants/antiplatelets concomitantly
Epidemiologic studies on bone fracture risk following exposure to some antidepressants, including SSRIs, have reported an association between antidepressant treatment and fractures; there are multiple possible causes for this observation and it is unknown to what extent fracture risk is directly attributable to SSRI treatment
Bone fractures reported to be associated with antidepresant use
Consider risk of serotonin syndrome if administered concomitantly with other serotonergic drugs including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, amphetamines, and St. John’s Wort
Sexual dysfunction
- Use may cause symptoms of sexual dysfunction in both male and female patients; inform patients that they should discuss any changes in sexual function and potential management strategies with their healthcare provider
- Use of SSRIs, may cause symptoms of sexual dysfunction; in male patients, SSRI use may result in ejaculatory delay or failure, decreased libido, and erectile dysfunction
- In female patients, SSRI/SNRI use may result in decreased libido and delayed or absent orgasm
- Important for prescribers to inquire about sexual function prior to initiation of therapy and to inquire specifically about changes in sexual function during treatment, because sexual function may not be spontaneously reported
- When evaluating changes in sexual function, obtaining a detailed history (including timing of symptom onset) is important because sexual symptoms may have other causes, including underlying psychiatric disorder
- Discuss potential management strategies to support patients in making informed decisions about treatment
Pregnancy & Lactation
Pregnancy
Pregnancy category: D
Teratogenic effects: Epidemiologic studies have shown that infants exposed to paroxetine in the first trimester of pregnancy have an increased risk of congenital malformations, particularly cardiovascular malformations
Use late in the third trimester associated with complications in newborns and may require prolonged hospitalization, respiratory support, and tube feeding
A study of nearly 28,000 women taking SSRIs confirmed 5 previously reported birth defercts associated with paroxetine, including heart defects, anencephaly, and abdominal wall defects (BMJ 2015; 351:h3190)
Persistent pulmonary hypertension of the newborn
- Potential risk of persistent pulmonary hypertension of the newborn (PPHN) when used during pregnancy
- Initial public health advisory in 2006 was based on a single published study; since then, there have been conflicting findings from new studies, making it unclear whether use of SSRIs during pregnancy can cause PPHN
- FDA has reviewed the additional new study results and has concluded that, given the conflicting results from different studies, it is premature to reach any conclusion about a possible link between SSRI use in pregnancy and PPHN
- FDA recommendation: FDA advises health care professionals not to alter their current clinical practice of treating depression during pregnancy and to report any adverse events to the FDA MedWatch program
- A meta-analysis of 7 observational studies, found exposure to SSRIs in late pregnancy (ie, >20 weeks' gestation) more than doubled the risk of PPHN that could not be explained by other etiologies (eg, congenital malformations, meconium aspiration) (BMJ 2014;348:f6932)
Lactation
Excreted in breast milk; use caution (AAP states effect on nursing infants is unknown but may be of concern)
Pregnancy Categories
A: Generally acceptable. Controlled studies in pregnant women show no evidence of fetal risk.
B: May be acceptable. Either animal studies show no risk but human studies not available or animal studies showed minor risks and human studies done and showed no risk. C: Use with caution if benefits outweigh risks. Animal studies show risk and human studies not available or neither animal nor human studies done. D: Use in LIFE-THREATENING emergencies when no safer drug available. Positive evidence of human fetal risk. X: Do not use in pregnancy. Risks involved outweigh potential benefits. Safer alternatives exist. NA: Information not available.Pharmacology
Mechanism of Action
SSRI; little or no affinity for alpha-adrenergic histamine or cholinergic receptor
Absorption
Peak plasma time: 5.2-8.1 hr (immediate-release); 6-10 hr (controlled-release)
Peak plasma concentration: 61.7 ng/mL
Distribution
Protein bound: 93-95%
Vd: 8.7 L/kg
Metabolism
Metabolism: Hepatic P450 enzyme CYP2D6
Enzymes inhibited: CYP2D6
Metabolites: Inactive
Elimination
Half-life: 21 hr
Dialyzable: No
Excretion: Urine (64%); feces (36%)
Pharmacogenomics
Several SSRIs (eg, fluoxetine, fluvoxamine, paroxetine, sertraline) are metabolized by CYP2D6
CYP2D6 is involved in the metabolism of approximately 20% of drugs in clinical use, and it displays large individual-to-individual variability in activity due to genetic polymorphisms
More than 80 CYP2D6 variant alleles have been identified; however, 4 of the most prevalent alleles, CYP2D6*3, *4, *5, and *6, account for 93-97% of CYP2D6 poor metabolizers (PMs)
CYP2D6*4, the most common variant (~25% frequency in whites), causes a splicing defect; CYP2D6*3 (2.7% frequency) causes a frameshift mutation; and CYP3D6*5 (2.6%) is an entire deletion of the CYP2D6 gene; individuals homozygous for these alleles have no CYP2D6 activity
The impact of CYP2D6 activity is further complicated in some SSRIs (eg, fluoxetine, fluvoxamine, paroxetine, sertraline) that in addition to being substrates for CYP2D6, are also known to moderately inhibit CYP2D6 activity
Genetic testing laboratories
- Genotyping tests for CYP2D6 variants are commercially available through the following companies
- Applied Biosystems (http://www.appliedbiosystems.com/)
- GenPath Diagnostics (http://www.genpathdiagnostics.com/)
Images
| BRAND | FORM. | UNIT PRICE | PILL IMAGE |
|---|---|---|---|
| Paxil oral - | 10 mg/5 mL suspension |  | |
| Paxil oral - | 40 mg tablet | 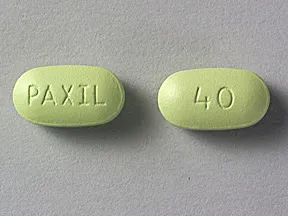 | |
| Paxil oral - | 20 mg tablet |  | |
| Paxil oral - | 10 mg tablet |  | |
| Paxil oral - | 30 mg tablet | 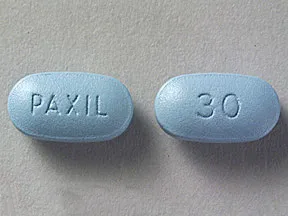 | |
| Paxil oral - | 10 mg tablet |  | |
| paroxetine oral - | 10 mg tablet | 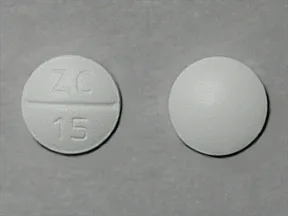 | |
| paroxetine oral - | 37.5 mg tablet |  | |
| paroxetine oral - | 30 mg tablet |  | |
| paroxetine oral - | 20 mg tablet | 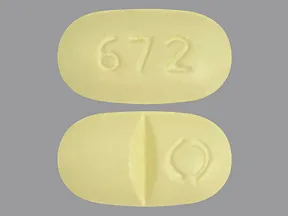 | |
| paroxetine oral - | 30 mg tablet |  | |
| paroxetine oral - | 20 mg tablet | 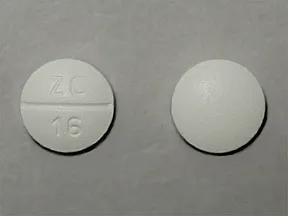 | |
| paroxetine oral - | 10 mg tablet |  | |
| paroxetine oral - | 25 mg tablet | 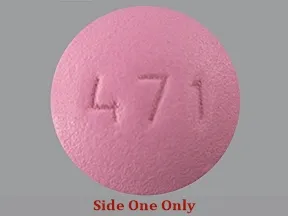 | |
| paroxetine oral - | 12.5 mg tablet | 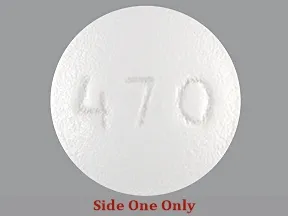 | |
| paroxetine oral - | 40 mg tablet | 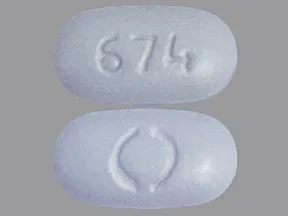 | |
| paroxetine oral - | 30 mg tablet | 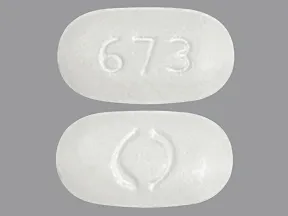 | |
| paroxetine oral - | 10 mg tablet |  | |
| paroxetine oral - | 20 mg tablet | 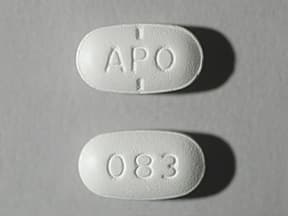 | |
| paroxetine oral - | 25 mg tablet |  | |
| paroxetine oral - | 12.5 mg tablet |  | |
| paroxetine oral - | 40 mg tablet | 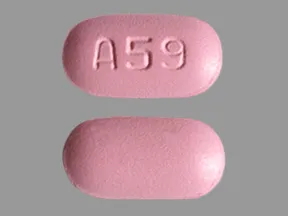 | |
| paroxetine oral - | 40 mg tablet |  | |
| paroxetine oral - | 30 mg tablet |  | |
| paroxetine oral - | 20 mg tablet | 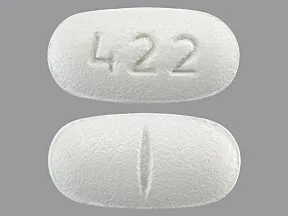 | |
| paroxetine oral - | 10 mg tablet |  | |
| paroxetine oral - | 25 mg tablet |  | |
| paroxetine oral - | 12.5 mg tablet |  | |
| paroxetine oral - | 12.5 mg tablet | 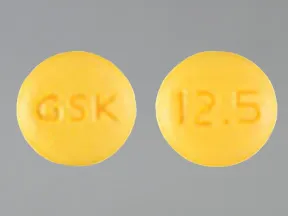 | |
| paroxetine oral - | 20 mg tablet |  | |
| paroxetine oral - | 30 mg tablet |  | |
| paroxetine oral - | 37.5 mg tablet |  | |
| paroxetine oral - | 20 mg tablet |  | |
| paroxetine oral - | 30 mg tablet |  | |
| paroxetine oral - | 10 mg tablet |  | |
| paroxetine oral - | 40 mg tablet |  | |
| paroxetine oral - | 40 mg tablet |  | |
| paroxetine oral - | 37.5 mg tablet |  | |
| paroxetine oral - | 40 mg tablet | 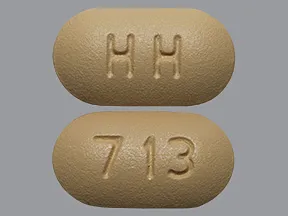 | |
| paroxetine oral - | 20 mg tablet |  | |
| paroxetine oral - | 40 mg tablet |  | |
| paroxetine oral - | 20 mg tablet |  | |
| paroxetine oral - | 10 mg tablet |  | |
| paroxetine oral - | 10 mg tablet |  | |
| paroxetine oral - | 37.5 mg tablet | 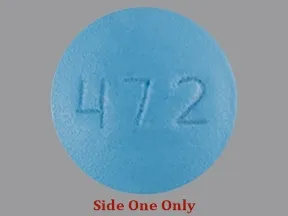 | |
| paroxetine oral - | 40 mg tablet |  | |
| paroxetine oral - | 25 mg tablet | 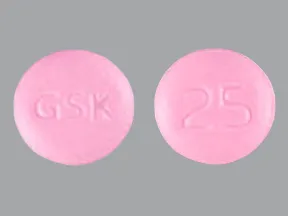 | |
| paroxetine oral - | 37.5 mg tablet |  | |
| paroxetine oral - | 30 mg tablet |  | |
| paroxetine oral - | 25 mg tablet |  | |
| paroxetine oral - | 12.5 mg tablet |  | |
| paroxetine oral - | 30 mg tablet |  | |
| paroxetine oral - | 10 mg tablet | 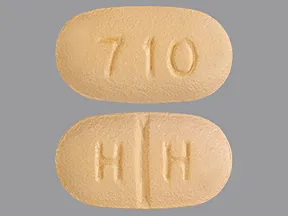 | |
| paroxetine oral - | 37.5 mg tablet |  | |
| paroxetine oral - | 25 mg tablet |  | |
| paroxetine oral - | 37.5 mg tablet |  | |
| paroxetine oral - | 20 mg tablet |  | |
| paroxetine oral - | 12.5 mg tablet |  | |
| Paxil CR oral - | 37.5 mg tablet |  | |
| Paxil CR oral - | 25 mg tablet | 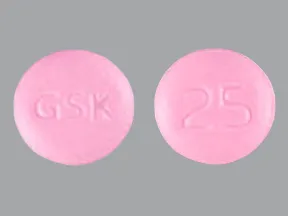 | |
| Paxil CR oral - | 37.5 mg tablet |  | |
| Paxil CR oral - | 25 mg tablet | 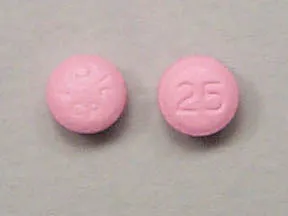 | |
| Paxil CR oral - | 12.5 mg tablet |  | |
| Paxil CR oral - | 25 mg tablet |  |
Copyright © 2010 First DataBank, Inc.
Patient Handout
paroxetine oral
PAROXETINE CONTROLLED-RELEASE - ORAL
(pa-ROX-e-teen)
COMMON BRAND NAME(S): Paxil CR
WARNING: Antidepressant medications are used to treat a variety of conditions, including depression and other mental/mood disorders. These medications can help prevent suicidal thoughts/attempts and provide other important benefits. However, studies have shown that a small number of people (especially people younger than 25) who take antidepressants for any condition may experience worsening depression, other mental/mood symptoms, or suicidal thoughts/attempts. It is very important to talk with the doctor about the risks and benefits of antidepressant medication (especially for people younger than 25), even if treatment is not for a mental/mood condition.Tell the doctor right away if you notice worsening depression/other psychiatric conditions, unusual behavior changes (including possible suicidal thoughts/attempts), or other mental/mood changes (including new/worsening anxiety, panic attacks, trouble sleeping, irritability, hostile/angry feelings, impulsive actions, severe restlessness, very rapid speech). Be especially watchful for these symptoms when a new antidepressant is started or when the dose is changed.
USES: This medication is used to treat certain mental/mood disorders (such as depression, panic attacks, anxiety disorders). It is also used to treat a severe form of premenstrual syndrome (premenstrual dysphoric disorder). Paroxetine belongs to a class of drugs known as selective serotonin reuptake inhibitors (SSRIs). It works by helping to restore the balance of a certain natural substance (serotonin) in the brain.
HOW TO USE: Read the Medication Guide and, if available, the Patient Information Leaflet provided by your pharmacist before you start taking paroxetine and each time you get a refill. If you have any questions, ask your doctor or pharmacist.Take this medication by mouth with or without food as directed by your doctor, usually once daily in the morning. Taking this medication with food may decrease nausea. If this medication makes you sleepy during the day, talk to your doctor about taking it in the evening. Swallow the tablets whole. Do not crush or chew the tablets. Doing so can release all of the drug at once, increasing the risk of side effects.The dosage is based on your medical condition, response to treatment, age, and other medications you may be taking. Be sure to tell your doctor and pharmacist about all the products you use (including prescription drugs, nonprescription drugs, and herbal products). To reduce your risk of side effects, your doctor may start you at a low dose and gradually increase your dose. Follow your doctor's instructions carefully. Do not increase your dose or use this drug more often or for longer than prescribed. Your condition will not improve any faster, and your risk of side effects will increase. Take this medication regularly to get the most benefit from it. To help you remember, take it at the same time each day.If you are taking paroxetine for premenstrual problems, your doctor may direct you to take it every day of the month or just for the 2 weeks before your period through the first full day of your period.Keep taking this medication even if you feel well. Do not stop taking this medication without consulting your doctor. Some conditions may become worse when this drug is suddenly stopped. Also, you may experience symptoms such as mood swings, headache, tiredness, sleep changes, and brief feelings similar to electric shock. To prevent these symptoms while you are stopping treatment with this drug, your doctor may reduce your dose gradually. Consult your doctor or pharmacist for more details. Report any new or worsening symptoms right away.It may take up to several weeks before you get the full benefit of this drug.Tell your doctor if your condition does not improve or if it worsens.
SIDE EFFECTS: See also Warning section.Nausea, drowsiness, dizziness, trouble sleeping, loss of appetite, weakness, dry mouth, sweating, blurred vision, and yawning may occur. If any of these effects last or get worse, tell your doctor or pharmacist promptly.Remember that this medication has been prescribed because your doctor has judged that the benefit to you is greater than the risk of side effects. Many people using this medication do not have serious side effects.Tell your doctor right away if you have any serious side effects, including: shaking (tremor), restlessness, inability to keep still, decreased interest in sex, changes in sexual ability, numbness/tingling, easy bleeding/bruising, fast/irregular heartbeat, muscle weakness/spasm, seizures.Get medical help right away if you have any very serious side effects, including: black stools, vomit that looks like coffee grounds, eye pain/swelling/redness, widened pupils, vision changes (such as seeing rainbows around lights at night).This medication may increase serotonin and rarely cause a very serious condition called serotonin syndrome/toxicity. The risk increases if you are also taking other drugs that increase serotonin, so tell your doctor or pharmacist of all the drugs you take (see Drug Interactions section). Get medical help right away if you develop some of the following symptoms: fast heartbeat, hallucinations, loss of coordination, severe dizziness, severe nausea/vomiting/diarrhea, twitching muscles, unexplained fever, unusual agitation/restlessness.Rarely, males may have a painful or prolonged erection lasting 4 or more hours. If this occurs, stop using this drug and get medical help right away, or permanent problems could occur.A very serious allergic reaction to this drug is rare. However, get medical help right away if you notice any symptoms of a serious allergic reaction, including: rash, itching/swelling (especially of the face/tongue/throat), severe dizziness, trouble breathing.This is not a complete list of possible side effects. If you notice other effects not listed above, contact your doctor or pharmacist.In the US -Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 or at www.fda.gov/medwatch.In Canada - Call your doctor for medical advice about side effects. You may report side effects to Health Canada at 1-866-234-2345.
PRECAUTIONS: Before taking paroxetine, tell your doctor or pharmacist if you are allergic to it; or if you have any other allergies. This product may contain inactive ingredients, which can cause allergic reactions or other problems. Talk to your pharmacist for more details.Before using this medication, tell your doctor or pharmacist your medical history, especially of: personal or family history of bipolar/manic-depressive disorder, personal or family history of suicide attempts, liver problems, kidney problems, seizures, low sodium in the blood, bleeding problems, personal or family history of glaucoma (angle-closure type).This drug may make you dizzy or drowsy or blur your vision. Alcohol or marijuana (cannabis) can make you more dizzy or drowsy. Do not drive, use machinery, or do anything that needs alertness or clear vision until you can do it safely. Avoid alcoholic beverages. Talk to your doctor if you are using marijuana (cannabis).Before having surgery, tell your doctor or dentist about all the products you use (including prescription drugs, nonprescription drugs, and herbal products).Older adults may be more sensitive to the side effects of this drug, especially bleeding or loss of coordination. Older adults may also be more likely to develop a type of salt imbalance (hyponatremia), especially if they are also taking "water pills" (diuretics). Loss of coordination can increase the risk of falling.Children may be more sensitive to the side effects of this drug, especially loss of appetite and weight loss. Monitor weight and height in children who are taking this drug.This medication is not recommended for use during pregnancy. It may harm an unborn baby, and babies born to mothers who have used it during the last 3 months of pregnancy may sometimes develop withdrawal symptoms such as feeding/breathing difficulties, seizures, muscle stiffness, or constant crying. However, since untreated mental/mood problems (such as depression, panic attack, obsessive-compulsive disorder, and anxiety) can harm a pregnant woman and her unborn baby, do not stop taking this medication unless directed by your doctor. Instead, ask your doctor if a different medication would be right for you. If you are planning pregnancy, become pregnant, or think you may be pregnant, tell your doctor right away.This drug passes into breast milk. Consult your doctor before breastfeeding.
DRUG INTERACTIONS: Drug interactions may change how your medications work or increase your risk for serious side effects. This document does not contain all possible drug interactions. Keep a list of all the products you use (including prescription/nonprescription drugs and herbal products) and share it with your doctor and pharmacist. Do not start, stop, or change the dosage of any medicines without your doctor's approval.Some products that may interact with this drug are: thioridazine, other drugs that can cause bleeding/bruising (including antiplatelet drugs such as clopidogrel, NSAIDs such as ibuprofen/naproxen, "blood thinners" such as dabigatran/warfarin).Aspirin can increase the risk of bleeding when used with this medication. However, if your doctor has directed you to take low-dose aspirin for heart attack or stroke prevention (usually 81-162 milligrams a day), you should continue taking it unless your doctor instructs you otherwise. Ask your doctor or pharmacist for more details.This medication can slow down the removal of other medications from your body, which may affect how they work. Examples of affected drugs include atomoxetine, phenothiazines, pimozide, risperidone, tamoxifen, tetrabenazine, antiarrhythmics such as propafenone/flecainide, TCA antidepressants such as desipramine/amitriptyline, among others.Taking MAO inhibitors with this medication may cause a serious (possibly fatal) drug interaction. Avoid taking MAO inhibitors (isocarboxazid, linezolid, metaxalone, methylene blue, moclobemide, phenelzine, procarbazine, rasagiline, safinamide, selegiline, tranylcypromine) during treatment with this medication. Most MAO inhibitors should also not be taken for two weeks before and after treatment with this medication. Ask your doctor when to start or stop taking this medication.The risk of serotonin syndrome/toxicity increases if you are also taking other drugs that increase serotonin. Examples include street drugs such as MDMA/"ecstasy," St. John's wort, certain antidepressants (including other SSRIs such as citalopram/fluoxetine, SNRIs such as duloxetine/venlafaxine), tryptophan, among others. The risk of serotonin syndrome/toxicity may be more likely when you start or increase the dose of these drugs.Tell your doctor or pharmacist if you are taking other products that cause drowsiness including alcohol, marijuana (cannabis), antihistamines (such as cetirizine, diphenhydramine), drugs for sleep or anxiety (such as alprazolam, diazepam, zolpidem), muscle relaxants, and opioid pain relievers (such as codeine).Check the labels on all your medicines (such as allergy or cough-and-cold products) because they may contain ingredients that cause drowsiness. Ask your pharmacist about using those products safely.This medication may interfere with certain medical/lab tests (such as brain scan for Parkinson's disease), possibly causing false test results. Make sure lab personnel and all your doctors know you use this drug.
OVERDOSE: If someone has overdosed and has serious symptoms such as passing out or trouble breathing, call 911. Otherwise, call a poison control center right away. US residents can call their local poison control center at 1-800-222-1222. Canada residents can call a provincial poison control center. Symptoms of overdose may include: irregular heartbeat, fainting, severe dizziness, seizures.
NOTES: Do not share this medication with others.Keep all regular medical and psychiatric appointments.
MISSED DOSE: If you miss a dose, take it as soon as you remember. If it is near the time of the next dose, skip the missed dose. Take your next dose at the regular time. Do not double the dose to catch up.
STORAGE: Store at room temperature away from light and moisture. Do not store in the bathroom. Keep all medications away from children and pets.Do not flush medications down the toilet or pour them into a drain unless instructed to do so. Properly discard this product when it is expired or no longer needed. Consult your pharmacist or local waste disposal company.
Information last revised March 2024. Copyright(c) 2024 First Databank, Inc.
IMPORTANT: HOW TO USE THIS INFORMATION: This is a summary and does NOT have all possible information about this product. This information does not assure that this product is safe, effective, or appropriate for you. This information is not individual medical advice and does not substitute for the advice of your health care professional. Always ask your health care professional for complete information about this product and your specific health needs.
Formulary
Adding plans allows you to compare formulary status to other drugs in the same class.
To view formulary information first create a list of plans. Your list will be saved and can be edited at any time.
Adding plans allows you to:
- View the formulary and any restrictions for each plan.
- Manage and view all your plans together – even plans in different states.
- Compare formulary status to other drugs in the same class.
- Access your plan list on any device – mobile or desktop.





